Sleep apnea is a serious sleep disorder that affects breathing during sleep. While many people have heard of sleep apnea, fewer understand that there are different types and that each type has different causes, risks, and treatment approaches. The two most commonly discussed forms are obstructive sleep apnea and central sleep apnea.
In this article, we will clearly explain the key differences between obstructive and central sleep apnea, using simple language so you can understand what’s happening in the body, how symptoms differ, and why correct diagnosis is important.
What Is Sleep Apnea?
Sleep apnea is a condition where breathing repeatedly stops and starts while a person is sleeping. These pauses in breathing reduce oxygen levels in the body and force the brain to wake the person briefly to restart breathing. These awakenings usually happen without the person realizing it, but they prevent deep, restful sleep.
Over time, untreated sleep apnea can increase the risk of heart disease, high blood pressure, stroke, diabetes, and daytime exhaustion.
Understanding Obstructive Sleep Apnea
Obstructive sleep apnea, often called OSA, is the most common type of sleep apnea. It happens when the airway becomes physically blocked during sleep.
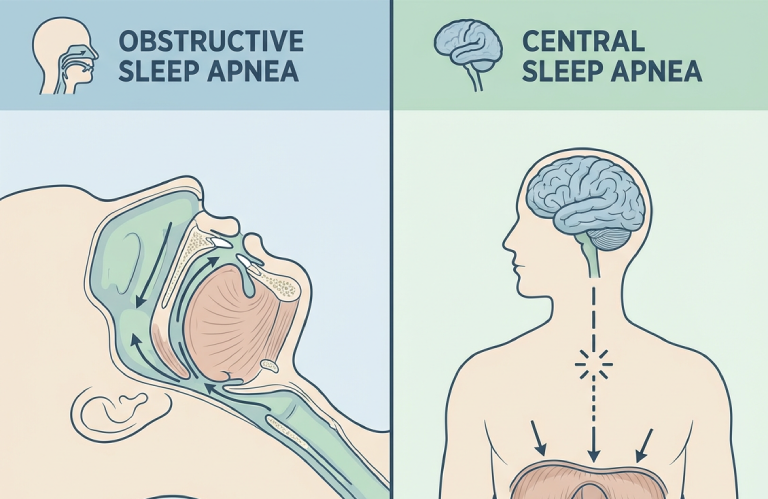
When a person falls asleep, the muscles in the throat relax. In people with obstructive sleep apnea, these muscles relax too much, causing the airway to narrow or collapse. As a result, air cannot flow properly into the lungs, even though the body is trying to breathe.
Common causes of obstructive sleep apnea include excess weight, a narrow airway, large tonsils, jaw structure issues, and relaxed throat muscles. Loud snoring is one of the most noticeable signs of this condition.
Understanding Central Sleep Apnea
Central sleep apnea is less common and very different in how it occurs. Instead of a blocked airway, central sleep apnea happens when the brain does not send the correct signals to the muscles that control breathing.
In this case, there is no physical blockage in the throat. The airway remains open, but breathing stops because the brain temporarily “forgets” to tell the body to breathe. This type of sleep apnea is often linked to neurological or medical conditions.
Central sleep apnea may be associated with heart failure, stroke, brain injuries, or certain medications that affect breathing control.
Obstructive vs Central Sleep Apnea: How They Differ
The main difference between obstructive and central sleep apnea lies in the cause of breathing pauses. Obstructive sleep apnea is a physical problem, while central sleep apnea is a communication problem between the brain and the body.
In obstructive sleep apnea, breathing efforts continue but airflow is blocked. In central sleep apnea, there is little or no breathing effort because the brain does not send the signal to breathe.
Snoring is usually loud and common in obstructive sleep apnea, while it may be mild or absent in central sleep apnea. However, both conditions cause repeated oxygen drops and sleep disruptions.
Symptoms: What Patients May Experience
Both types of sleep apnea share some similar symptoms, but there are differences in how they present.
People with obstructive sleep apnea often experience loud snoring, choking or gasping during sleep, morning headaches, dry mouth, and extreme daytime sleepiness. Bed partners often notice breathing pauses first.
Central sleep apnea symptoms may include frequent nighttime awakenings, shortness of breath during sleep, insomnia, and fatigue. Snoring may not always be present, making the condition harder to notice.
In both cases, poor sleep quality can lead to mood changes, difficulty concentrating, and reduced quality of life.
Why Proper Diagnosis Is Important
Correctly identifying whether a person has obstructive or central sleep apnea is critical because treatment approaches differ. Treating the wrong type may not improve symptoms and could delay proper care.
Sleep studies are the main diagnostic tool. These tests monitor breathing patterns, oxygen levels, brain activity, and heart rate during sleep. The results help doctors determine which type of sleep apnea is present and how severe it is.
Dental professionals may also play a role in identifying obstructive sleep apnea, especially when jaw alignment, teeth grinding, or airway structure contribute to the condition.
Treatment Differences Between the Two Types
Treatment for obstructive sleep apnea often focuses on keeping the airway open during sleep. This may include lifestyle changes, oral appliances, or other therapies designed to improve airflow.
Oral appliance therapy is commonly used in dental sleep medicine and can be highly effective for many patients with obstructive sleep apnea. These devices gently reposition the jaw to prevent airway collapse.
Central sleep apnea treatment focuses more on addressing the underlying medical or neurological condition. In some cases, specialized breathing devices or medical management may be required to stabilize breathing patterns during sleep.
Can Someone Have Both Types?
Yes, some individuals experience a combination of both obstructive and central sleep apnea. This condition is sometimes referred to as complex or mixed sleep apnea.
In these cases, a person may initially have obstructive sleep apnea and later develop central sleep apnea, especially after starting certain treatments. Managing this condition usually requires close medical supervision and a personalized treatment plan.
Why Early Detection Matters
Both obstructive and central sleep apnea can have serious long-term health consequences if left untreated. Early detection allows patients to receive the right treatment, improve sleep quality, and reduce health risks.
Many people notice significant improvements in energy, focus, mood, and overall well-being once sleep apnea is properly managed.
Final Thoughts
Understanding the difference between obstructive vs central sleep apnea helps patients make informed decisions about their health. While both conditions disrupt breathing during sleep, their causes, symptoms, and treatments are not the same.
If you or someone you care about experiences persistent sleep problems, loud snoring, breathing pauses, or constant fatigue, professional evaluation is essential. The right diagnosis is the first step toward safer sleep and better health.